- Report: #155696
Complaint Review: Humana Health Insurance - Louisville Kentucky
Humana Health Insurance dishonest Louisville Kentucky
*Consumer Comment: Humana not dishonest, you just need to know the questions to ask
*REBUTTAL Individual responds: 9/11/05 Rebuttal to Humana Dishonest
*REBUTTAL Individual responds: 9/11/05 Rebuttal to Humana Dishonest
*REBUTTAL Individual responds: 9/11/05 Rebuttal to Humana Dishonest
*Consumer Suggestion: He did ask the right question
*UPDATE Employee: Always go by what's in writing.
*Author of original report: Rebuttal to Always Go What is in Writing
*Author of original report: Rebuttal to Always Go What is in Writing
*Author of original report: Rebuttal to Always Go What is in Writing
*Consumer Suggestion: Hard to determine.
*Consumer Suggestion: Hard to determine.
*Consumer Suggestion: Hard to determine.
*Consumer Suggestion: Hard to determine.
*Consumer Comment: Hard to determine
*Consumer Suggestion: What?
*Consumer Comment: No, I don't think the provider asked for "benefits"
*Consumer Suggestion: Where?
*Consumer Comment: The client asked how much the copay was
*Consumer Suggestion: Fact versus Opinion
*Consumer Comment: Read the post
*Consumer Comment: Read the post
*Consumer Comment: Read the post
*Consumer Comment: Read the post
*Consumer Suggestion: You weren't there.
*Consumer Comment: I'm sorry, you must be right-
*Consumer Suggestion: A difference.
*Consumer Comment: Sorry probably won't butter the buscuit
*Consumer Suggestion: Easy answer
*Consumer Comment: Please read complaints before posting
*UPDATE Employee: not alot of detail
John
Woodlawn, Kentucky
U.S.A.
30 Updates & Rebuttals
Humanarep
your mom''''s house,New Mexico,
USA
not alot of detail
#2UPDATE Employee
Wed, March 17, 2010
There's not a lot of detail here, but it sounds like you asked for an office visit benefit, but the provider probably billed for an office surgery or something. That's usually a deductible driven service on most employer plans.
Franzg
Cincinnati,Ohio,
U.S.A.
Please read complaints before posting
#3Consumer Comment
Thu, June 04, 2009
That way you won't get as frustrated. I honestly believe Humana made an error by giving incorrect information on the telephone. It caused this client to lose money. The client feels "ripped off". I also believe there may be instances when a client is given proper information on the phone. There may actually be good employees at Humana. Unfortunately, you will not find that information posted on ripoff report.
I Am The Law
Cincinnati,Ohio,
U.S.A.
Easy answer
#4Consumer Suggestion
Wed, June 03, 2009
Easy answer:The claim came in for something different than what the member asked about. How is this Humana's fault? Oh, I forgot. My friend Franzg thinks that Humana has fortune tellers on call. Get real, Franzg. I suppose you'd blame the conflict in the Middle East on this company. Your small mind is boring me and I'm tired of trying to educate a small mind. I'm done with you.
Franzg
Cincinnati,Ohio,
U.S.A.
Sorry probably won't butter the buscuit
#5Consumer Comment
Sat, May 23, 2009
"However, when I received my Statement of Benefits outlining a $500.00 co-pay, I immediately made and specifically documented my third call to Humana informing me again of a $25.00 co-pay." Doesn't sound like OP asked for "a different procedure". Humana wins again.
I Am The Law
Cincinnati,Ohio,
U.S.A.
A difference.
#6Consumer Suggestion
Fri, May 22, 2009
It sounds like the claim came in for different services that what you originally asked about. Sorry that happened to you?
Franzg
Cincinnati,Ohio,
U.S.A.
I'm sorry, you must be right-
#7Consumer Comment
Mon, April 20, 2009
How deluded I must be to actually believe the original complaint. How silly of me to think that a Humana employee would give incorrect information to this client. How narrow minded of me to think Humana could be in error! OMG! Let's all expand our minds, and understand that this victim must be lying. The advice we give should be "stop lying". I think you should start explaining to everyone why you think the client would lie on this site. Then your advice would be relevant. Right now, your advice is pretty useless. I think the proper advice would be to tell the client to complain. In Humana's terms a complaint is a "grievance and appeal", which must be in writing, and mailed to a PO Box in Kentucky. Otherwise, the client would be arrested for filing an "illegal" complaint. Heaven forbid! Making a phone call to file a complaint. Totally "against the law". This is a silly law everybody. Please understand that the bureaucracy and waste inherent in the managed care system is costing us $640 billion a year. Its too much. Managed care needs to do better, or just disappear. As for working for managed care, I would never work for a corporation which makes errors frequently, and gets everybody else to pay for them. It just isn't worth it. Now go back to your job, and start raising our premiums to help Humana's "bottom" line.
I Am The Law
Cincinnati,Ohio,
U.S.A.
You weren't there.
#8Consumer Suggestion
Wed, April 15, 2009
'I immediately made and specifically documented my third call to Humana informing me again of a $25.00 co-pay.' Just because you wrote something down doesn't make it true. Franzg said that "I have no reason to doubt the integrity of this victim of deception". What a closed mind. He wasn't on the call yet comments like he was... don't listen to this person. He works for a rival insurance carrier.
Franzg
Cincinnati,Ohio,
U.S.A.
Read the post
#9Consumer Comment
Tue, April 14, 2009
"I immediately made and specifically documented my third call to Humana informing me again of a $25.00 co-pay." You should flame the original poster if you don't believe them. I have no reason to doubt the integrity of this victim of deception.
Franzg
Cincinnati,Ohio,
U.S.A.
Read the post
#10Consumer Comment
Tue, April 14, 2009
"I immediately made and specifically documented my third call to Humana informing me again of a $25.00 co-pay." You should flame the original poster if you don't believe them. I have no reason to doubt the integrity of this victim of deception.
Franzg
Cincinnati,Ohio,
U.S.A.
Read the post
#11Consumer Comment
Tue, April 14, 2009
"I immediately made and specifically documented my third call to Humana informing me again of a $25.00 co-pay." You should flame the original poster if you don't believe them. I have no reason to doubt the integrity of this victim of deception.
Franzg
Cincinnati,Ohio,
U.S.A.
Read the post
#12Consumer Comment
Tue, April 14, 2009
"I immediately made and specifically documented my third call to Humana informing me again of a $25.00 co-pay." You should flame the original poster if you don't believe them. I have no reason to doubt the integrity of this victim of deception.
I Am The Law
Cincinnati,Ohio,
U.S.A.
Fact versus Opinion
#13Consumer Suggestion
Mon, April 13, 2009
Ok Franzg, How do you know what the patient asked when they were confirming benefits? Were you on the phone? No, you were not. You're talking about people you don't know anything about and about a situation you don't know about, so you're far from an authority. You're so quick to say "Humana screwed up", well maybe it was the patient not asking the correct questions, or perhaps the claim was filed differently than the benefits the patient asked about. (Obviously this would be beyond the Humana rep's control.) Since you work for a managed care facility yourself, I'd think you'd understand.
Franzg
Cincinnati,Ohio,
U.S.A.
The client asked how much the copay was
#14Consumer Comment
Sat, March 14, 2009
Humana employee replied "$25" Client was misled. Humana employee failed to reply correctly- correct response is "I do not know". Client cannot complain verbally. Must find PO Box # in Kentucky. If YOU want to complain, I suggest you call Humana Customer "care" at 800-448-6262, since you claim that's how Humana fields complaints. Instead of ripping on clients for not reading a "certificate", maybe you should educate Humana employees how to properly respond to client questions. I think to be fair, you need to blast the Humana employee for not understanding a simple question. After all, we are not all perfect and so well educated about healthcare and the intricacies of corporate law. Cut us some slack every once in a while. I'm sorry you are angry about the posts. I think it may help individuals in our democracy to understand the reality about how our healthcare dollars are spent. I'm also sorry you object to me and my opinion, and feel it necessary to attempt to find out "where" I work. I guess you assume I am an employee of some kind.
I Am The Law
Cincinnati,Ohio,
U.S.A.
Where?
#15Consumer Suggestion
Fri, March 13, 2009
So Franzg, where do you work so I can post a bunch of hateful and false reports about them online?
Franzg
Cincinnati,Ohio,
U.S.A.
No, I don't think the provider asked for "benefits"
#16Consumer Comment
Wed, March 11, 2009
I think the consumer asked the carrier how much their co-pay would be. Perhaps you should read the consumer's complaint before posting. Perhaps the Humana employee should have replied "I do not know- do you expect me to predict the future? after all, I am not Nostradamus" instead of "$25" when the request was made. No, I don't expect any accurate predictions. I only expect to be treated with dignity and respect when I donate a chunk of my monthly salary for a worthless "healthcare certificate" and having to put up with employees who fabricate figures to tell their clients.
I Am The Law
Cincinnati,Ohio,
U.S.A.
What?
#17Consumer Suggestion
Wed, March 11, 2009
Franzg, again???? So, you think it's the carrier's fault when a provider asks for benefits for one thing and then sends in a claim for something else different later on? Ok.... hmmm. Oh, I forgot. You think that insurance carriers can predict the future. My bad. Well, let's think about this one, Nostradamus: Insurance carriers can not guarantee benefits on a claim they don't have. Duh. I'd like to think that that's common sense, but from the insane rantings of certain people on ROR, I guess it's not.
Franzg
Cincinnati,Ohio,
U.S.A.
Hard to determine
#18Consumer Comment
Fri, February 27, 2009
Yes, Humana has no idea what the claim was going to be. So why did they mislead the client? Why not just cut these jerks out of the loop. They "don't know" how much they are willing to pay until they have already misled you. Your physician probably knew. I would suggest dealing with the physicians directly, and avoid the inaccuracy and indecisiveness of corporations like Humana. Though their job is tough, they are a touted "fortune 500" corporation. I would expect accuracy about how much my insurance would pay for a medical procedure. It seems Humana could have it together enough to at least have a complaints department (like one with an actual telephone). The client could iron out these problems before posting on ripoff report. It just seems easier for a consumer to get an estimate, then explore options about how to cover the costs. Also, to be able to seek a more realistic option if necessary. What is wrong with that? Instead, we pay a large corporation to dictate our choices. It essentially "owns" our healthcare contracts. Managed care is dysfunctional, and a waste.
I Am The Law
Cincinnati,Ohio,
U.S.A.
Hard to determine.
#19Consumer Suggestion
Fri, February 20, 2009
I read your story and I think what's happening here is that the way the claim was billed was different from the benefits you called in about. (Honestly, without seeing the claim and Humana's call documentation, that's impossible to determine.) Here's an example of what I'm talking about: if you went into a doctor's office to get a thorn taken out of your hand, you might call into Humana and ask them what your office visit benefits would be. Now, when the claim came into Humana, the doctor may have billed for a minor outpatient surgery. Believe me, I see that constantly. It's no one's fault per se, and I'm not trying to take up for Humana, but they can't predict the future. They can quote benefits for you, but who knows what's going to show up on the claim when they actually get it?
I Am The Law
Cincinnati,Ohio,
U.S.A.
Hard to determine.
#20Consumer Suggestion
Fri, February 20, 2009
I read your story and I think what's happening here is that the way the claim was billed was different from the benefits you called in about. (Honestly, without seeing the claim and Humana's call documentation, that's impossible to determine.) Here's an example of what I'm talking about: if you went into a doctor's office to get a thorn taken out of your hand, you might call into Humana and ask them what your office visit benefits would be. Now, when the claim came into Humana, the doctor may have billed for a minor outpatient surgery. Believe me, I see that constantly. It's no one's fault per se, and I'm not trying to take up for Humana, but they can't predict the future. They can quote benefits for you, but who knows what's going to show up on the claim when they actually get it?
I Am The Law
Cincinnati,Ohio,
U.S.A.
Hard to determine.
#21Consumer Suggestion
Fri, February 20, 2009
I read your story and I think what's happening here is that the way the claim was billed was different from the benefits you called in about. (Honestly, without seeing the claim and Humana's call documentation, that's impossible to determine.) Here's an example of what I'm talking about: if you went into a doctor's office to get a thorn taken out of your hand, you might call into Humana and ask them what your office visit benefits would be. Now, when the claim came into Humana, the doctor may have billed for a minor outpatient surgery. Believe me, I see that constantly. It's no one's fault per se, and I'm not trying to take up for Humana, but they can't predict the future. They can quote benefits for you, but who knows what's going to show up on the claim when they actually get it?
I Am The Law
Cincinnati,Ohio,
U.S.A.
Hard to determine.
#22Consumer Suggestion
Fri, February 20, 2009
I read your story and I think what's happening here is that the way the claim was billed was different from the benefits you called in about. (Honestly, without seeing the claim and Humana's call documentation, that's impossible to determine.) Here's an example of what I'm talking about: if you went into a doctor's office to get a thorn taken out of your hand, you might call into Humana and ask them what your office visit benefits would be. Now, when the claim came into Humana, the doctor may have billed for a minor outpatient surgery. Believe me, I see that constantly. It's no one's fault per se, and I'm not trying to take up for Humana, but they can't predict the future. They can quote benefits for you, but who knows what's going to show up on the claim when they actually get it?
John
Woodlawn,Kentucky,
U.S.A.
Rebuttal to Always Go What is in Writing
#23Author of original report
Wed, November 14, 2007
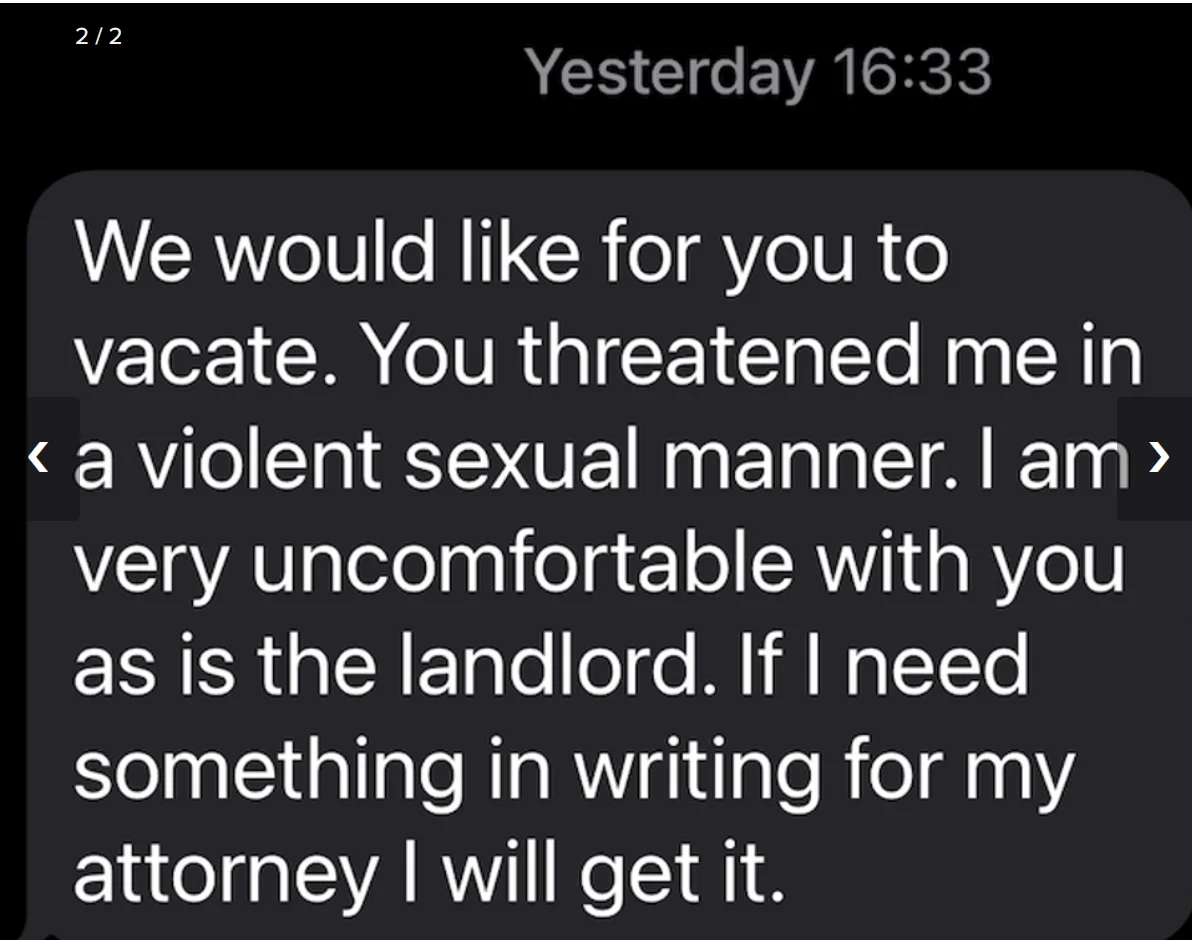
Thank you for the more recent rebuttal, though my complaint to me seems distant now. In terms of going what was in writing, I did, though it was not specific to the particular procedure. So I expected the higher co-pay, and I was surprised when Humana twice told me over the phone, before and after my procedure, the lower co-pay applied. After complaining, Humana had supposedly no documentation of my first call, and the representative I documented on my second call supposedly denied what she told me. My resolution to my complaints through Humana and then the BBB was for Humana to simply acknowledge the discrepancies of what they were communicating over the phone, which Humana would not do. John Woodlawn, KY USA
John
Woodlawn,Kentucky,
U.S.A.
Rebuttal to Always Go What is in Writing
#24Author of original report
Wed, November 14, 2007
Thank you for the more recent rebuttal, though my complaint to me seems distant now. In terms of going what was in writing, I did, though it was not specific to the particular procedure. So I expected the higher co-pay, and I was surprised when Humana twice told me over the phone, before and after my procedure, the lower co-pay applied. After complaining, Humana had supposedly no documentation of my first call, and the representative I documented on my second call supposedly denied what she told me. My resolution to my complaints through Humana and then the BBB was for Humana to simply acknowledge the discrepancies of what they were communicating over the phone, which Humana would not do. John Woodlawn, KY USA
John
Woodlawn,Kentucky,
U.S.A.
Rebuttal to Always Go What is in Writing
#25Author of original report
Wed, November 14, 2007
Thank you for the more recent rebuttal, though my complaint to me seems distant now. In terms of going what was in writing, I did, though it was not specific to the particular procedure. So I expected the higher co-pay, and I was surprised when Humana twice told me over the phone, before and after my procedure, the lower co-pay applied. After complaining, Humana had supposedly no documentation of my first call, and the representative I documented on my second call supposedly denied what she told me. My resolution to my complaints through Humana and then the BBB was for Humana to simply acknowledge the discrepancies of what they were communicating over the phone, which Humana would not do. John Woodlawn, KY USA
Amy
Taylorsville,Kentucky,
U.S.A.
Always go by what's in writing.
#26UPDATE Employee
Sat, November 03, 2007
News flash - customer service reps can be wrong. On average, customer service reps at Humana, I'm told, have four minutes to take a call and answer the consumer's question. It's entirely possible that they misunderstood your question, pulled up the wrong screen in what I know first-hand is an incredibly confusing database system, or something of that nature. Does that stink? Sure. People make mistakes. Customer service at an insurance company is, I imagine, a very stressful job. This, however, is why the company provides you with written information, via the Web and by request, about your particular benefits. You can view an explanation of your benefits on the Website in PDF format, which I highly recommend doing since you clearly have an Internet connection. Odds are, as a prior person explained, you were given the office copay, not the surgery copay. As a benefits specialist, I can tell you that inpatient and surgical copays are often much higher than office visit copays. Now, if you look up your written documentation and it clearly states your surgical copay is not $500, you have a legitimate argument and you should try to escalate the problem. But always, ALWAYS go by what's in writing, not by what someone tells you. It's more reliable, and then you also have documentation to back your assertions.
Mike
Radford,Virginia,
U.S.A.
He did ask the right question
#27Consumer Suggestion
Sun, September 11, 2005
He must have asked something like "How much will this procedure end up costing me out of pocket?" And the company told him $25.00, but now they want $500.00. It's a rip-off. File a complaint with the state, but I'm sure they've heard it all before.
John
Woodlawn,Kentucky,
U.S.A.
9/11/05 Rebuttal to Humana Dishonest
#28REBUTTAL Individual responds
Sun, September 11, 2005
This is in response to the 9/11/05 Rebuttal from North Hollywood, CA. The rebuttal misses the whole point of my complaint. I was told one thing by Humana over the phone, which Humana denied telling me over the phone. And Humana falsely documented my phone calls. John Woodlawn, KY USA
John
Woodlawn,Kentucky,
U.S.A.
9/11/05 Rebuttal to Humana Dishonest
#29REBUTTAL Individual responds
Sun, September 11, 2005
This is in response to the 9/11/05 Rebuttal from North Hollywood, CA. The rebuttal misses the whole point of my complaint. I was told one thing by Humana over the phone, which Humana denied telling me over the phone. And Humana falsely documented my phone calls. John Woodlawn, KY USA
John
Woodlawn,Kentucky,
U.S.A.
9/11/05 Rebuttal to Humana Dishonest
#30REBUTTAL Individual responds
Sun, September 11, 2005
This is in response to the 9/11/05 Rebuttal from North Hollywood, CA. The rebuttal misses the whole point of my complaint. I was told one thing by Humana over the phone, which Humana denied telling me over the phone. And Humana falsely documented my phone calls. John Woodlawn, KY USA
Deone
North Hollywood,California,
U.S.A.
Humana not dishonest, you just need to know the questions to ask
#31Consumer Comment
Sun, September 11, 2005
If you would look at your policy, it would tell you that your co-pay is $25 for a Dr's visit. A Dr's visit is just that, not an operation. If you had an operation and all you had to spend was $500 consider yourself lucky. I sell health insurance and I know it spells it out. 25 for office visit, a specialist is 40. Hospital stays and surgery is after your deductible and subject to co-insurance, and on some major things there maybe additional co-pays.